Hereditary pancreatitis
If you tested your DNA with a personal genomics service like 23andMe, AncestryDNA, FamilyTreeDNA, MyHeritage or another testing company, you can learn more about your risk factors for hundreds of diseases. By clicking the button above ⬆️, you can upload your raw DNA data file and receive a personalized 250-page health report with research links that is the most comprehensive.
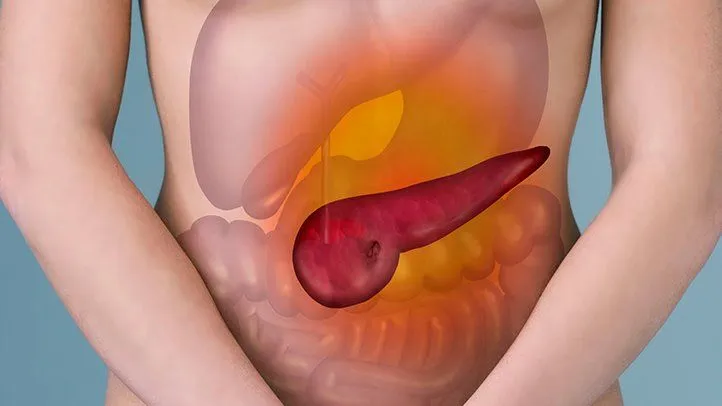
Pancreatitis is a multifaceted ailment that can stem from various sources. If pancreatitis arises in several closely related individuals, it necessitates additional scrutiny, which may involve genetic counseling and/or genetic testing. To diagnose hereditary or familial pancreatitis, a 3-generation family history must be gathered, and other potential causes of pancreatitis in the family (such as gallstones, excessive alcohol consumption, or cystic fibrosis) must be evaluated. Genetic testing can assist in determining whether hereditary or familial pancreatitis is present in a family. Despite their similar names, these two diagnoses have significant distinctions.
Pancreatitis may arise from various causes such as medications, infections, trauma, autoimmune disease or lifestyle factors, but it can also be attributed to genetic factors.
The main culprit behind hereditary pancreatitis is the presence of variations in the PRSS1 gene. Nonetheless, not all families afflicted with this condition can trace it back to a genetic cause in the PRSS1 gene. It is approximated that 60% to 85% of individuals with hereditary pancreatitis can pinpoint a genetic cause. For those without a disease-causing variation in PRSS1, other genes, some of which remain unidentified, can trigger hereditary pancreatitis.
Instructions for producing the digestive enzyme cationic trypsinogen, which assists in food digestion, are provided by the PRSS1 genes and synthesized in the pancreas.
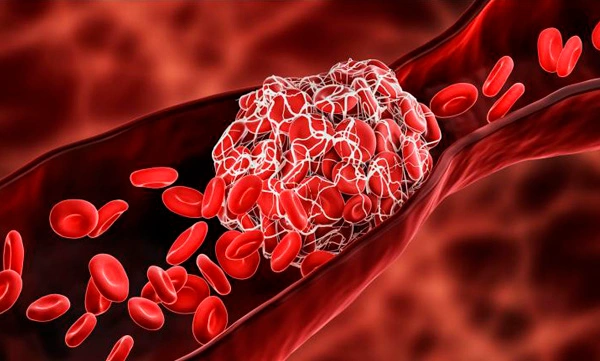
According to the U.S. National Library of Medicine, certain mutations in the PRSS1 gene can lead to hereditary pancreatitis by causing the premature conversion of a cationic trypsinogen enzyme to trypsin within the pancreas. Alternatively, other mutations can prevent the breakdown of trypsin, resulting in increased levels of the enzyme in the pancreas. This elevated trypsin activity can harm pancreatic tissue and incite an immune response, leading to inflammation in the pancreas.
The reason why some individuals with a disease-causing variant in PRSS1 do not develop hereditary pancreatitis is still unclear. However, it has been estimated that about 80% of those with a variant in the PRSS1 gene are likely to develop pancreatitis.
The condition of hereditary pancreatitis is intriguing and has shed light on the pathophysiology of pancreatitis. Nevertheless, there remain numerous unresolved inquiries, particularly regarding the connection between these mutations and pancreatitis and cancer. It is crucial that a team of skilled pancreatic specialists, capable of providing genetic counseling, oversee the care of these patients. To enhance management strategies and advance genetic research, it is imperative that patients be registered with one of the major Hereditary Pancreatitis Registries.
Follow the link of the selected polymorphism to read a brief description of how the selected polymorphism affects Pancreatitis and see a list of existing studies.
SNP polymorphisms related to the topic Pancreatitis:
| rs111033565 | rs111033565(A) is the most common mutation found in early (childhood) acute recurrent pancreatitis or chronic pancreatitis. |
| rs10273639 | PRSS1-PRSS2 variants encoding trypsin influence the risk of asparaginase-related pancreatitis. |
| rs17107315 | Mutations in the pancreatic secretory trypsin inhibitor gene (PSTI/SPINK1), are strongly associated with pancreatitis. |
| rs5751901 | Gamma-glutamyltransferase gene variation causes risk of chronic pancreatitis as well as acute pancreatitis in smokers. |
| rs111033566 | A novel cationic trypsinogen (PRSS1) cause autosomal dominant hereditary pancreatitis. |
| rs12688220 | A common variant of the MORC4 gene accounts for the predisposition to the disease in patients with chronic pancreatitis. |
| rs193922659 | Variants of a signalling peptide that disrupts pancreatic secretory trypsin inhibitor (SPINK1) secretion cause hereditary autosomal dominant pancreatitis. |
| rs11319 | |
| rs213950 | |
| rs225320 | |
| rs928302 | |
| rs4705202 | |
| rs5751902 | |
| rs10436957 | |
| rs11548596 | |
| rs121909293 | |
| rs121909294 | |
| rs144422014 | |
About The Author
Li DaliLi Dali, a National Foundation for Outstanding Youth Fund recipient, is a researcher at the School of Life Sciences in East China Normal University. He earned his PhD in genetics from Hunan Normal University in 2007 and conducted collaborative research at Texas A&M University during his doctoral studies. Li Dali and his team have optimized and innovated gene editing technology, leading to the establishment of a world-class system for constructing gene editing disease models.